Disc herniations are normally a further development of a previously existing disc “protrusion”, a condition in which the outermost layers of the annulus fibrosus are still intact, but can bulge when the disc is under pressure. In contrast to a herniation, none of the nucleus pulposus escapes beyond the outer layers.
Factors that lead to slipped disc include aging with associated degeneration and loss of elasticity of the discs and supporting structures; Poor posture combined with the habitual use of incorrect body mechanics, hard physical labour (delivery), improper lifting, especially if accompanied by twisting or turning; excessive strain, and sudden forceful trauma. A herniation may develop suddenly or gradually over weeks or months.
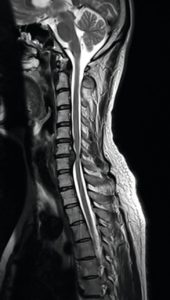
Herniated discs can occur in any part of the spine. Herniated discs are more common in the lower back especially at the L4-L5 and L5-S1 levels (lumbar disc herniation). This is because the lumbar spine carries most of the body’s weight. The second most common area is neck (cervical disc herniation). The area in which you experience pain depends on what part of the spine is affected.
The progression to an actual Herniation varies from slow to sudden onset of symptoms. There are four stages:
- disc protrusion
- prolapsed disc
- disc extrusion
- sequestered disc
Stages 1 and 2 are referred to as incomplete, where 3 and 4 are complete herniations. Pain resulting from herniation may be combined with a radiculopathy, which means neurological deficit. The deficit may include sensory changes (i.e. tingling, numbness) and/or motor changes (i.e. weakness, reflex loss). These changes are caused by nerve compression created by pressure from interior disc material.
People between the ages of 30 and 50 appear to be vulnerable because the elasticity and water content of the nucleus decreases with age. But of late it is seen that even the people around age group 20 – 30 are also getting affected with slip disc, because of their life style, stress and diet habits.
Symptoms of a herniated disc can vary depending on the location of the herniation and the types of soft tissue that become involved. They can range from little or no pain if the disc is the only tissue injured, to severe and unrelenting neck or low back pain that will radiate into the regions served by affected nerve roots that are irritated or impinged by the herniated material.
Often, herniated discs are not diagnosed immediately, as the patients come with undefined pains in the thighs, knees, or feet. Other symptoms may include sensory changes such as numbness, tingling, muscular weakness, paralysis, paresthesia, and affection of reflexes. If the herniated disc is in the lumbar region the patient may also experience sciatica due to irritation of one of the nerve roots of the sciatic nerve. Patients with L3 or L5 herniated disc (usually affecting the knee and leg) also have a high chance of experiencing decreased sexual performance (erectile dysfunction).
Unlike a pulsating pain or pain that comes and goes which can be caused by muscle spasm, pain from a herniated disc is usually continuous or at least is continuous in a specific position of the body.
It is possible to have a herniated disc without any pain or noticeable symptoms, depending on its location. If the extruded nucleus pulposus material doesn’t press on soft tissues or nerves, it may not cause any symptoms.
Typically, symptoms are experienced only on one side of the body. If the prolapse is very large and presses on the spinal cord or the cauda equina in the lumbar region, affection of both sides of the body may occur, often with serious consequences. Compression of the cauda equina can cause permanent nerve damage or paralysis. The nerve damage can result in loss of bowel and bladder control as well as sexual dysfunction. This disorder is called cauda equina syndrome.
A herniated disc can therefore produce symptoms anywhere along the course of that nerve, though the injury and irritation of the nerve are at the spine itself (referred pain). A slipped disc can produce different symptoms like varying degrees of pain in the back or neck along with numbness or weakness, tingling, Paralysis of single muscles, possibly with pain radiating to the arms or legs, paralysis in the part of the body below the spinal cord pressure, disturbance of feeling in the limbs, muscle spasms, difficulty controlling bowel movements or bladder function, disturbance of feeling in the rectum and the inside of the thighs etc,.
Diagnosis is made by a Doctor based on your history, symptoms, a physical examination, and results of tests, including the following:
- X-ray: Application of radiation to produce a film or picture of a part of the body can show the structure of the vertebrae and the outline of the joints. X-rays of the spine are obtained to search for other potential causes of pain, i.e. tumors, infections, fractures, etc.
- Computed tomography scan (CT or CAT scan): A diagnostic image created after a computer reads x-rays; can show the shape and size of the spinal canal, its contents, and the structures around it.
- Magnetic resonance imaging (MRI): A diagnostic test that produces three-dimensional images of body structures using powerful magnets and computer technology; can show the spinal cord, nerve roots, and surrounding areas, as well as enlargement, degeneration, and tumors.
- Myleogram: An x-ray of the spinal canal following injection of a contrast material into the surrounding cerebrospinal fluid spaces; can show pressure on the spinal cord or nerves due to herniated discs, bone spurs or tumors.
- Electromyogram and Nerve Conduction Studies (EMG/NCS): These tests measure the electrical impulse along nerve roots, peripheral nerves, and muscle tissue. This will indicate whether there is ongoing nerve damage, if the nerves are in a state of healing from a past injury, or whether there is another site of nerve compression.
Ayurveda Management of Slip disc

At CHARAKA, we are providing very effective and most successful treatment for Slip disc or herniated disc. With our vast experience in treating Spine related conditions, today we are successfully dealing even post surgical recurrence cases.
The treatment comprises of Detoxification and rejuvenation through Ayurvedic Panchakarma therapy, administration of researched medicines internally.
The therapies like Abyanga swedam, Nasyam, Pathrapotala swedam, Choornapinda swedam, Pizhichil, Shirodhara, Kadeevasthy, Greevavasthy, Navarakizhi, Vasti etc. are done as per the necessity and condition. These therapies are directed towards relieving the inflammatory changes, releasing the spasms and nerve compressions in the affected area, strengthening the supportive tissues holding the spine, nourishing the joints through improving the circulation. Usually the treatment period is 4 – 5 weeks according to the severity of the disease.
In four to six weeks, the majority of patients find their symptoms are relieved, without surgery. If patient can come for the treatment in early stages, even total cure without recurrence is also possible.

