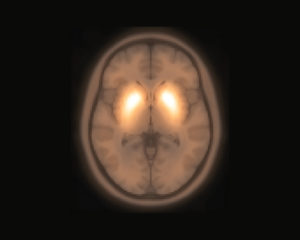
 Parkinson’s disease (PD) is a degenerative disorder of the central nervous system. The motor symptoms of Parkinson’s disease result from the death of dopamine-generating cells in the substantia nigra, a region of the midbrain; the cause of this cell death is unknown. Early in the course of the disease, the most obvious symptoms are movement-related; these include shaking, rigidity, slowness of movement and difficulty with walking and gait. Later, cognitive and behavioral problems may arise, with dementia commonly occurring in the advanced stages of the disease. Other symptoms include sensory, sleep and emotional problems.
Parkinson’s disease (PD) is a degenerative disorder of the central nervous system. The motor symptoms of Parkinson’s disease result from the death of dopamine-generating cells in the substantia nigra, a region of the midbrain; the cause of this cell death is unknown. Early in the course of the disease, the most obvious symptoms are movement-related; these include shaking, rigidity, slowness of movement and difficulty with walking and gait. Later, cognitive and behavioral problems may arise, with dementia commonly occurring in the advanced stages of the disease. Other symptoms include sensory, sleep and emotional problems.
Parkinson’s disease is often defined as a ‘Parkinsonian syndrome’ that is idiopathic (having no known cause), although some atypical cases have a genetic origin.
The progression of Parkinson’s disease and the degree of impairment vary from individual to individual. Many people with Parkinson’s disease live long productive lives, whereas others become disabled much more quickly. Premature death is usually due to complications such as falling-related injuries or pneumonia.
Parkinson’s disease is a heterogeneous and genetically complex disorder of largely unknown etiology. It is the second most common neurodegenerative disease in the general population. Approximately four million people worldwide are estimated to be living with Parkinson’s disease. Incidence of Parkinson’s increases with age, but an estimated four percent of people with PD are diagnosed before the age of 50. Adult-onset Parkinson’s disease is most common, but early-onset Parkinson’s disease (onset between 21-40 years), and juvenile-onset Parkinson’s disease (onset before age 21) also exist.
Modern treatments are effective at managing the early motor symptoms of the disease, mainly through the use of levodopa and dopamine agonists. As the disease progresses and dopaminergic neurons continue to be lost, these drugs eventually become ineffective at treating the symptoms and at the same time produce a complication called dyskinesia, marked by involuntary writhing movements. Diet and some forms of rehabilitation have shown some effectiveness at alleviating symptoms. Surgery and deep brain stimulation have been used to reduce motor symptoms as a last resort in severe cases where drugs are ineffective.
Classification
The term Parkinsonism is used for a motor syndrome whose main symptoms are tremor at rest, stiffness, slowing of movement and postural instability. The main motor symptoms are collectively called “Parkinsonism” or “Parkinsonian syndrome”. Parkinsonian syndromes can be divided into four subtypes according to their origin:
- Primary or idiopathic
- Secondary or acquired,
- Hereditary Parkinsonism
- Parkinson plus syndrome
Parkinson’s disease is the most common form of Parkinsonism and is usually defined as “primary” Parkinsonism, meaning parkinsonism with no external identifiable cause.
Parkinson’s plus syndrome
Parkinson’s plus syndrome is the name for a group of neurological conditions that are very similar to Parkinson’s disease. Because these conditions cause symptoms that are very similar to Parkinson’s, they are often incorrectly diagnosed. However, these conditions can even be treated using many of the same medications and therapies as Parkinson’s.
Conditions that are considered Parkinson’s plus syndromes include:
-
Progressive Supranuclear Palsy (PSP)
This is the most common Parkinson’s plus syndrome. PSP causes trouble with balance and stability that can mimic Parkinson’s disease. Unlike Parkinson’s disease, people with PSP don’t experience tremors. They do have difficulty with eye movement and are likely to experience more trouble with speech, swallowing, and mood than people with Parkinson’s disease.
-
Multiple System Atrophy (MSA)
MSA is a progressive condition that affects your nervous system. It causes stiffness and loss of balance similarly to Parkinson’s disease. Over time, the effects of the disease on your nervous system can lead to difficulty with essential body functions such as digestion, breathing, and your heartbeat. It also causes more typical Parkinson’s symptoms, like shaking, stiffness, and problems with balance or speech.
-
Corticobasal Ganglionic Degeneration (CBGD)
This is the rarest of the four main types. CBGD is a condition that causes parts of your brain to become smaller. This causes many symptoms that overlap with Parkinson’s disease, such as tremors and balance problems. Over time, it also can effect your ability to think, see, and speak clearly. As the disease gets worse, it gets harder to walk and swallow.
-
Lewy Body Dementia (LBD)
This is the second most common form of dementia after Alzheimer’s disease. LBD is a progressive brain condition caused by structures called Lewy bodies that form in your brain. People with LBD might have symptoms that resemble Parkinson’s disease, dementia, or a combination of both. It affects your ability to think clearly, speak, and remember things. It can make you confused and cause hallucinations. The symptoms get worse over time.
Signs and symptoms
The primary symptoms of Parkinson’s disease are all related to voluntary and involuntary motor function and usually start on one side of the body. Symptoms are mild at first and will progress over time. Some individuals are more affected than others. Studies have shown that by the time that primary symptoms appear, individuals with Parkinson’s disease will have lost 60% to 80% or more of the dopamine-producing cells in the brain.
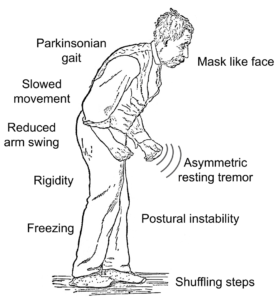
Characteristic motor symptoms include the following:
- Tremors: Trembling in fingers, hands, arms, feet, legs, jaw, or head. Tremors most often occur while the individual is resting, but not while involved in a task. Tremors may worsen when an individual is excited, tired, or stressed.
- Rigidity: Stiffness of the limbs and trunk, which may increase during movement. Rigidity may produce muscle aches and pain. Loss of fine hand movements can lead to cramped handwriting (micrographia) and may make eating difficult.
- Bradykinesia: Slowness of voluntary movement. Over time, it may become difficult to initiate movement and to complete movement. Bradykinesia together with stiffness can also affect the facial muscles and result in an expressionless, “mask-like” appearance.
- Postural instability: Impaired or lost reflexes can make it difficult to adjust posture to maintain balance. Postural instability may lead to falls.
- Parkinsonian gait: Individuals with more progressive Parkinson’s disease develop a distinctive shuffling walk with a stooped position and a diminished or absent arm swing. It may become difficult to start walking and to make turns. Individuals may freeze in mid-stride and appear to fall forward while walking.
While the main symptoms of Parkinson’s disease are movement-related, progressive loss of muscle control and continued damage to the brain can lead to secondary symptoms. These vary in severity, and not every individual will experience all of them. Some of the secondary symptoms include:
- anxiety, insecurity, and stress
- depression
- confusion, memory loss, and dementia (more common in elderly individuals)
- Executive dysfunction, Slowed cognitive speed
- constipation
- insomnia, daytime drowsiness
- mask-like face expression
- small handwriting
- slowed, quieter speech, and monotone voice
- pain, paresthesia, Fatigue
- Dystonia (abnormal, sustained, painful twisting muscle contractions)
- difficulty in speech, swallowing and excessive salivation
- diminished sense of smell (hyposmia or anosmia)
- excessive sweating
- Altered sexual function
- skin problems, oily skin
- urinary incontinence
- Psychotic symptoms—hallucinations or delusions
- low blood pressure upon standing (orthostatic hypotension)
- blurred or double vision, decreased blink rate, dry eyes
Most people with Parkinson’s disease have idiopathic Parkinson’s disease (having no specific known cause). A small proportion of cases, however, can be attributed to known genetic factors. Other factors have been associated with the risk of developing PD, but no causal relationship has been proven.
An early and accurate diagnosis of Parkinson’s disease is important in developing good treatment strategies to maintain a high quality of life for as long as possible. A physician will diagnose Parkinson’s disease from the medical history and a neurological examination. There is no lab test that will clearly identify the disease, but brain scans and other laboratory tests are sometimes used to rule out disorders that could give rise to similar symptoms.
Patients may be given levodopa and resulting relief of motor impairment tends to confirm diagnosis. Individuals may sometimes be misdiagnosed as having another disorder, and sometimes individuals with Parkinson-like symptoms may be inaccurately diagnosed as having Parkinson’s disease. It is therefore important to re-evaluate individuals in the early phase on a regular basis to rule out other conditions that may be responsible for the symptoms.
The finding of Lewy bodies in the midbrain on autopsy is usually considered proof that the patient suffered from Parkinson’s disease.
Ayurveda Perspective & Management of Parkinson's disease

According to Ayurveda, most of the diseases of the Vata are essentially the conditions of degenerative diseases of the nervous system. Kampa vata is one such condition caused by imbalance of Vata. The treatment of ‘kampavata’ consists of both internal and external administration of drugs in different forms aimed to reverse the ‘vata’ imbalance.
Ayurveda was found to be an effective treatment for patients with Parkinson’s disease. Ayurveda is an ancient Indian system of medicine. It has an integrated approach to the prevention and treatment of illness and tries to maintain or re-establish the harmony between the mind, body, and forces of nature.
Several Scientific studies and clinical trials have revealed the effectiveness of Ayurveda herbs and preparations, also established the necessity of Ayurvedic cleansing procedures (Panchakarma Therapies) prior to the use of Palliative therapy.
At ‘CHARAKA’, we are offering exclusive Panchakarma therapies and researched internal medicines for treating Parkinson’s disease. These are found very effective not only in controlling the symptoms of PD but also in arresting the further progression of the disease. Quality of life can be improved drastically with these custom made therapies.
If the patient is already on Allopathic medication, these treatments and medicines can be comfortably combined with them. Our Ayurveda treatment regime proves effective in controlling the side effects of allopathic medications and even in reducing the dosage of allopathic medications.
If a patient can come in the initial stages or before starting the allopathic medication, the results are wonderful.

